Jan Van Berkel: The Fat Adapted Healthy Athlete
After transitioning to a low-carb, high-fat diet, professional Ironman athlete Jan Van Berkel not only recorded a personal best in the South African Ironman.

High levels of visceral fat, that is the fat we carry around our organs, is a well-known marker of health decay. Our athlete Jan Van Berkel experienced substantial reductions in visceral fat (339 g to 166 g) after making a few key changes in behavior. These adjustments coincided with large improvements in both health and performance, and just last week he recorded a personal best time in the South African Ironman (5th professional). Carry on reading to learn how he achieved this, and what it means to become a “F.A.H-lete”, or fat-adapted, healthy athlete.
The first major Ironman of the season for Plews and Prof athletes turned out to be a good one at Ironman South Africa (IMSA). With 4th and 5th places, and two personal best times from Kyle Buckingham and Jan Van Berkel (JVB). Both athletes delivered stellar performances on the day and were thrilled with their results.
I have been working with JVB since November last year. We started out working more on a consultancy basis, but since the new year has moved towards a coach-athlete relationship. JVB has been a pleasure to work with, and his result in IMSA was well deserved after a lot of hard work in training.
He managed to achieve this result even after training through a very cold winter in Switzerland, with limited biking and the ability to train outdoors. As many of us know, including Prof up in Canada, that isn’t easy!
When JVB and I first started working together, as with all athletes we work with, we begin with a battery of tests to establish some baseline parameters and monitor progress. One of the tests we used for JVB was a DEXA scan.
What is a DEXA scan?
DEXA stands for Dual-energy X-ray absorptiometry and is considered to be the gold standard tool for measuring body composition and bone mineral density. DEXA achieves this by using two X-ray beams of different energy levels, which are scanned up and down the body. When these different energy level photons pass through tissues, they slow at rates related to their elemental composition, and the unique elemental profiles of bone, fat, and non-bone lean tissue allow for visualization and determination of each tissue type.
In JVB’s case, we were interested in establishing baseline measures of his body composition, and specifically having a look at his level of fat mass relative to lean mass.

What is visceral fat and why is it more important than subcutaneous fat?
Visceral fat is excess intra-abdominal adipose tissue accumulation. In other words, it’s the fat that we can’t see, stored deep underneath the skin, rather than the subcutaneous fat that is more apparent to us on the outside of our body. The visceral (internal) fat is more of a gel-like fat that wraps around major organs, such as the liver, pancreas and kidneys. Having high levels of visceral fat has even led to a new term, called skinny-fat, referring to those who are thin on the outside, but fat on the inside. As you will discover, although some might not like it, it’s healthier to be thin on the inside and fat on the outside, although neither are that great.
Visceral fat is especially dangerous because these fat cells contribute to the way your body operates. Visceral fat is considered toxic and provokes inflammatory pathways. Such inflammation drives more fat deposition and interferes with the body’s normal hormonal functions. These changes can influence changes in appetite, fat gain, mood and brain function.
The Data
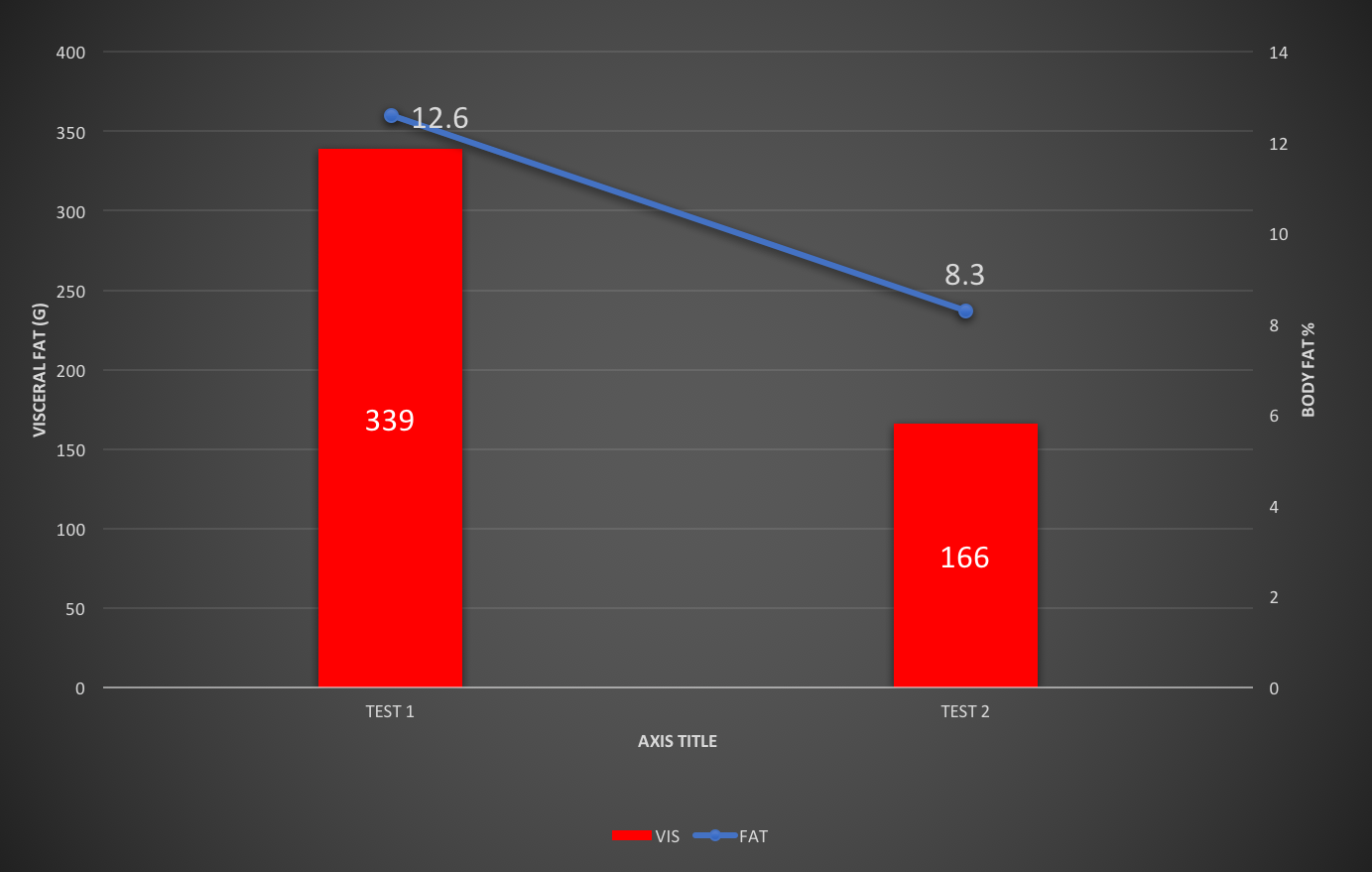
The DEXA scan data from JVB’s Test 1 and Test 2 (4 months apart) are shown above. To keep things simple, I have just included visceral fat and total body fat percentage. Visceral fat was cut nearly in half, going from 339 g to 166 g. As well, total body fat percentage was lowered from 12.6% to 8.3%.
Getting into science: how is this possible?
The changes in JVB’s visceral fat are quite remarkable, especially in an already lean elite athlete. From the outset, we should acknowledge that we don’t know exactly what mechanisms are responsible for the changes at this stage. However, using some guiding principles of physiology, we can make some reasonable assumptions. We would also like to give a massive thanks to our colleague Alessandro Ferretti for offering insights on the data as well.
After a lifetime of consuming the typical high carbohydrate diet prescribed to most endurance athletes, JVB likely had developed a mild to moderate level of insulin resistance (IR). Talking with Alessandro, who works with several high-level athletes, he’s noticed a relationship between competition level and IR; the higher the level, the more pronounced the IR problem. We have observed similar. The problem is, when we measure Hemoglobin A1c (HBA1c; aggregate blood glucose over 3 months, a marker of pre-diabetic state), we often get a false-negative result (i.e., no sign of any problem here). High training loads of course lower the blood glucose level, and we get lower HBA1c values over the long-term. While HBA1c values give us the false-negative result, morning fasted BG levels are likely to be raised.
We know that high blood glucose levels drive inflammation, and inflammation drives fat deposition. Typically, the inflammation will be magnified in a localized manner around both the gut and liver. In an athlete like Jan, who has very low levels of muscle fat and overall adiposity, a high(er) fat deposition around the organs can still be present as shown, as they remain inflamed due likely to IR and/or additional factors.
In endurance athletes undergoing high training loads (such as professional Ironman athletes), inflammation can be high, regardless of any IR, simply due to a chronically high training load. That, alongside a higher carbohydrate diet, means that inflammation never gets its chance to subside, even during periods of rest. We can assume that would be the case due to the link between training load, chronic glucocorticoid activation, inflammation and visceral fat deposition. Inflammation also appears to favor visceral over subcutaneous fat, meaning subcutaneous fat is the last place for inflammation to subside. Thus, fat remains hidden on the inside, as it was in JVB.
Another factor involved in excessive inflammation is that typically when we gain fat, we increase the number of fat cells (adipocytes). However, in such localized areas, rather than increasing the number of adipocytes, there seems to be an over-stretching of adipocyte fat deposition. This results in fat cells stretching over normal size, initiating a further inflammatory response that compounds the problem. Importantly, more inflammation under a high carbohydrate diet with IR, means more fat deposition around the organs.
When we consider all the above, high levels of visceral fat in some elite athletes may be apparent irrespective of any insulin resistance. This is due jointly to
- the exercise-induced inflammation alongside diets that are high in refined carbohydrates
- to the preference of inflammation to remain around the organs and
- to the overstretch/inflammation reaction that occurs when fat deposition around the organs is increased
Jan Van Berkel and Low Carb High Fat approach: how did it work?
So by now, the question I guess everyone is asking is: “how and why did JVB see such changes?” Very simply, a complete switch over to a low carbohydrate (CHO)/high fat (LCHF). JVB was very diligent in his diet, and didn’t take any shortcuts. Low carb for him was generally Ketonix device, and was able to ride for >4 hr. from fasted without any carbohydrate supplementation or the feeling of hunger. This is something he was previously unable to do.

JVB’s lower carb diet would likely have caused a cascade of events to occur. First, the diet allowed him to achieve a low and stable (non-fluctuating) blood glucose level. Second, he became more metabolically flexible. Improvements in metabolic flexibility resulted in an increase in the energy production derived from fat and ketones, which reduced the energy derived from external carbohydrate sources. Additionally, the reduction in blood glucose would have directly influenced his levels of inflammation, particularly around the organs. With visceral fat deposition reduced, the liver no longer has to work as hard to convert excess blood glucose into fat. As well, the shift in energy metabolism towards fat and ketones, means the cost of producing energy becomes lower, and reactive oxygen species (ROS) production is reduced. Less damage and inflammation during Jan’s training also occurs at the same energy equivalent. This again reduces the total inflammatory load and visceral fat deposition.
Due to the above mentioned factors, Jan Van Berkel achieved a massive 49% reduction in visceral fat.
Take home points
What is important here is that JVB had substantial improvements in his health by going away from the conventional high carb diet prescribed to most professional athletes. This occurred in concert with substantial improvements in his performance, which is difficult to argue against. Improvement in performance and health. As we’ve spoken on previously, fitness and health are NOT the same thing, and athletes with the wrong guidance can be even less healthy than your everyday working man or woman.
In the above case with Jan, a change in his diet may have played the pivotal role. However, in situations where athletes undergo chronic high-intensity training, the pivotal player may be the high-intensity exercise. Nevertheless, both are likely have an important part to play as previously discussed. The fat adapted healthy athlete is one who ticks both boxes, taking a holistic approach towards performance, health and longevity.


Comments ()